Abstract
Objective: Neonatal ankyloglossia is a subject of ongoing controversy among healthcare professionals. Our hypotheses were that ankyloglossia may cause ineffective latch onto the breast and nipple pain, leading to an early abandonment of breastfeeding, and that frenotomy decreased nipple pain and increased breastfeeding at discharge.
Design: Prospective cohort study.
Setting: Tertiary care hospital in Barcelona, Spain.
Participants: All the neonates born in our center in 2018.
Methods: We offered a frenotomy to all tongue-tied patients (Hazelbaker score ≤8 in appearance and/or ≤11 in function). We determined how many frenotomies we performed and whether breastfeeding improved in the short term. We compared the breastfeeding rates between treated and untreated tongue-tied and non tongue-tied neonates, and determined the effect of gender, birth mode, prematurity, birth weight and maternal age with multivariate logistic regression analyses.
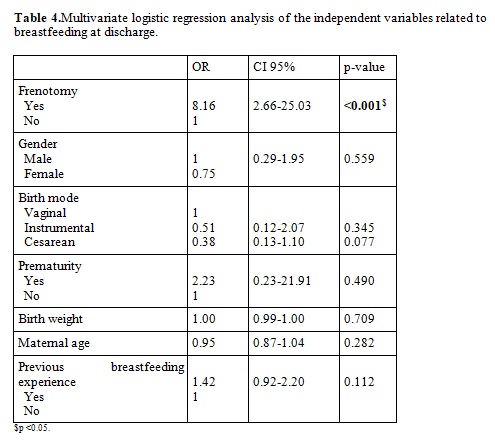
Results: Of the 1385 neonates born, 451 (32.5%, male to female ratio 1.4:1) were tongue-tied (mean Hazelbaker scores: 5.8 for appearance, 7.8 for function). Frenotomy was performed in 422 patients. The breastfeeding rate at discharge was higher among tongue-tied infants (92.1%) than non tongue-tied (84.2%), and higher among treated than untreated neonates (93.1 vs 75.9%, respectively). The protective effect of frenotomy continued regardless of the other variables analyzed in the multivariate logistic regression (OR 8.16, CI 95% 2.66-25.03).
Conclusion: Frenotomy is a simple, safe and effective procedure that may help increase the breastfeeding rate at discharge among tongue-tied neonates.
Keywords: ankyloglossia; nipple; frenotomy
COMPLET TEXT
Introduction:
The lingual frenulum is a submucosal band of connective tissue or a membrane that inserts on the tip of the tongue or along its undersurface (Hall & ; Renfrew, 2005; Ballard et al., 2002; Edmunds et al., 2011). We refer to ankyloglossia, or tongue-tie, when a thickened, tightened or shortened lingual frenulum restricts tongue movement (Hall & Renfrew, 2005; Ballard et al., 2002; Segal et al. 2007; Lalakea & Messner, 2003). The reported prevalence of ankyloglossia varies between less than 1% to 12.1% depending upon the study population and criteria used to define and grade ankyloglossia (Hall & Renfrew, 2005; Ballard et al., 2002; Edmunds et al., 2011; Segal et al., 2007; Messner et al., 2000; Hogan et al., 2005; Ricke et al., 2005). In a previous study we conducted, we observed a higher prevalence of ankyloglossia among our neonates born in 2018 (32.5%) (Maya-Enero et al., 2021).
Neonatal ankyloglossia is a subject of ongoing controversy among healthcare professionals. While some believe that it is rarely symptomatic, others believe that it may lead to several problems including early breastfeeding cessation. Even though the majority of tongue-tied infants are able to breastfeed, they are more likely to present poor latch onto the breast with resultant low milk transfer and failure to thrive and maternal nipple pain which may result in untimely weaning (Hall & Renfrew, 2005; Ballard et al., 2002; Edmunds et al., 2011; Messner et al., 2000; Knox, 2010; Haham et al., 2014). Some authors like Hogan and Ballard verified the positive effects of performing a frenotomy (Hall & Renfrew, 2005; Ballard et al., 2002; Edmunds et al., 2011; Segal et al. 2007; Lalakea & Messner, 2003; Messner & Lalakea, 2000; Rowan-Legg, 2015; Griffiths, 2004). More recently, Schlatter conducted a prospective, observational study that demonstrated frenotomy helpful in neonates with breastfeeding difficulties (Schlatter et al., 2019). Apart from ankyloglossia, other risk factors associated with unsuccessful breastfeeding include lack of breastfeeding experience, prematurity, low birth weight and being born by cesarean (Schlatter et al., 2019). Our hypotheses were that ankyloglossia can cause ineffective latch onto the breast and maternal nipple pain, leading to an early abandonment of breastfeeding, and that the surgical correction of tongue-ties in the first days decreases nipple pain in the short term and increases breastfeeding at discharge from the maternity ward at 48 to 72 hours after birth. Our objectives were to determine how often we performed a frenotomy and whether it improved breastfeeding in the short term in terms of maternal nipple pain or ineffective latch onto the breast, and if the breastfeeding rate was higher among surgically – treated Infants.
Patients and methods:
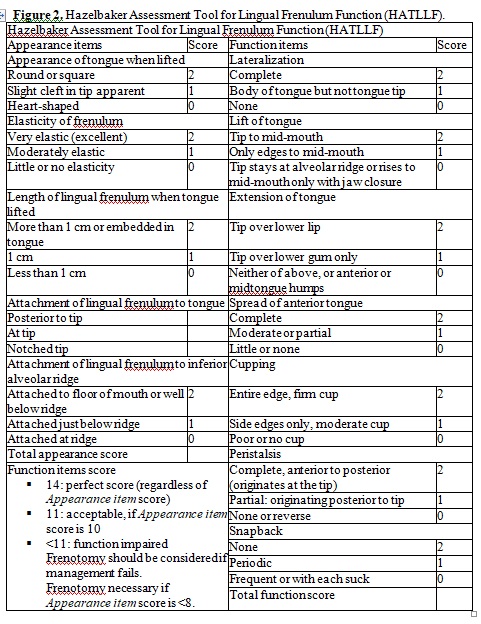
We conducted a prospective cohort study of the neonates born at a tertiary care hospital with an area of influence of about 400,000 people that experiences approximately 1,400 births per year. We included all the neonates born in our center between January 1 st and December 31 st 2018. We actively evaluated for the presence of ankyloglossia as part of the routine neonatal evaluation. At least one of the three staff neonatologists evaluated each patient. The examiner graded ankyloglossia based on Coryllos’s criteria (see Figure 1) (Coryllos et al., 2004). Apart from the prominence of the frenulum, we also assessed its impact on tongue appearance and function using the Hazelbaker score (Hazelbaker, 1993). A frenulum is symptomatic (thus, the patient is tongue-tied) if it scores 8 points or less in appearance and/or 11 points or less in function according to Hazelbaker (see Figure 2). Advice and help with positioning and latching onto the breast were given to all the mothers regardless of the presence of a tongue-tie and its treatment by IBCLC (International Board Certified Lactation Consultant) nurses before and after the frenotomy. We offered a frenotomy to all the tongue-tied patients if the mother had nipple pain or bruises or the neonate had problems latching onto the breast despite advice on correct positioning.
Frenotomy was performed by one of the three staff neonatologists if the parents accepted to. To perform a frenotomy, we wrap the baby in a towel, give it sucrose 24% as analgesia and let it suck for 2 minutes before the procedure. We use Coryllos’ technique, placing a sterile groove director under the tongue straddling the frenulum, holding the frenulum in place with visualization of tongue base and frenulum, and the frenulum is then snipped along the underside of the tongue to its base just proximal to the genioglossus muscle (Coryllos, 2004). We use the same technique in the case of submucosal tongue-ties (types 3 and 4), with dissection into the genioglossus muscle in the midline until a full release is achieved. We took into account the submucosal component of types 1 and 2. The area is checked to insure complete release. Following the frenotomy, we return the neonate to the mother for breastfeeding. At this time and until discharge from the maternity ward, we assess the quality of the infant’s latch onto the breast and maternal nipple pain. This is our standard practice for all the newborns. We recommend tongue rehabilitation exercises to be performed 8 to 10 times a day during the next month (see Figure 3). If frenotomy was performed, we assessed whether there was a short term improvement in breastfeeding by means of an immediate decrease of nipple pain and/or improved latch onto the breast taking into account the items in the LATCH breastfeeding charting system (Jensen, 1994). We collected demographic variables (gender, maternal age, birth weight, weight at discharge from the maternity ward, birth mode), the presence of ankyloglossia (and type of frenulum according to Coryllos), treatment for ankyloglossia, improvement after the frenotomy, and type of feed at discharge (breastfeeding, formula feeding, mixed feeding).
Our Ethics Committee approved the study (reference number: 2019/8537/I), which was conducted in accordance with the Declaration of Helsinki. Statistical analyses: Quantitative variables (gestational age, birth weight, weight at discharge), which were normally distributed, were described using the mean and standard deviation, and compared using a Student’s t-test. We compared the population of tongue- tied neonates (treated and untreated) with the total of neonates to verify that the samples
were homogeneous in terms of gestational age, birth weight and sex. Rates of breastfeeding between the three groups were compared using the Pearson chi square. Significance was set at the p < 0.05 level. Multivariate logistic regression analysis was used to determine the independent variables related to breastfeeding (frenotomy, gender, birth mode, prematurity,
birth weight, maternal age and previous breastfeeding experience). Results on these analyses were expressed as an odds ratio. For this analysis, we excluded neonates who were both breastfed and bottle-fed at the same time. To perform statistical analyses we used STATA version 15.1 (StataCorp, College Station, TX, USA).
Results:
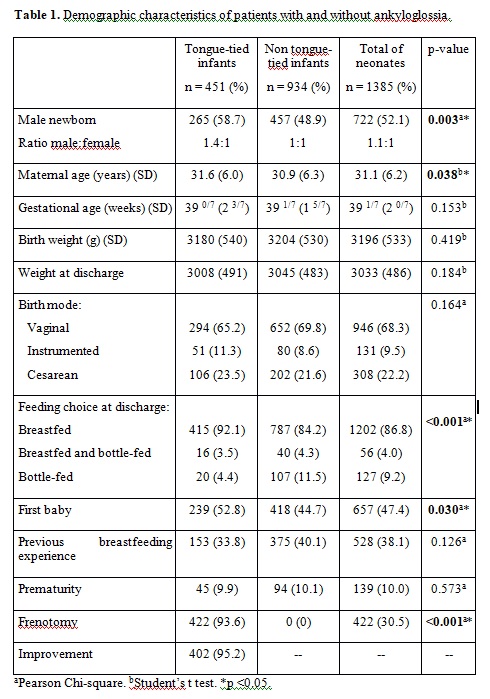
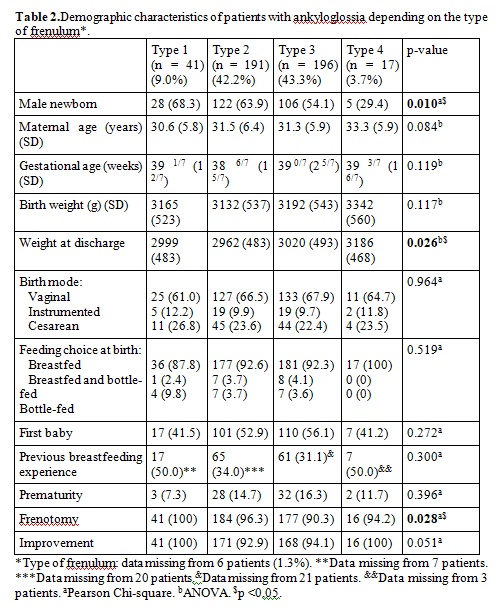
A total of 1392 neonates were born at our center in 2018. In this study, we included 1385 of them (99.5%) because we lacked information on 5 of the mothers. Of them, 451 (32.5%) had a tongue-tie. Tables 1 and 2 show the characteristics of the tongue-tied neonates vs non tongue-tied neonates and the subgroups of tongue-tied neonates. In 6 tongue-tied patients we could not find the type of frenulum they had according to Coryllos because that information lacked in their medical records. We also lacked the information on the rate of first baby or previous breastfeeding experience on 51 of the mothers as Table 2 shows. There were no differences in terms of mean gestational age (39 1/7 ± 2 0/7 weeks), birth weight (3196 ± 533 g), weight at discharge (3033 ± 486 g), weight loss, prematurity rate (10%) and birth mode (68.3% vaginal, 9.5% instrumented, 22.2% cesarean) between the groups in Tables 1 and 2. There were statistically significant differences in maternal age; however, the difference is not clinically relevant (31.6 vs 30.9 years). There were differences in gender: we found a male to female ratio of 1.4:1 (265 out of 451, 58.7%)
among tongue-tied neonates. We observed differences in the rate of first born: neonates with ankyloglossia were more likely to be first born (Table 1). The mean Hazelbaker score from tongue-tied infants was 5.8 points (SD 1.7, range 1-9) for appearance and 7.8 points (SD 1.8, range 1-13) for function.
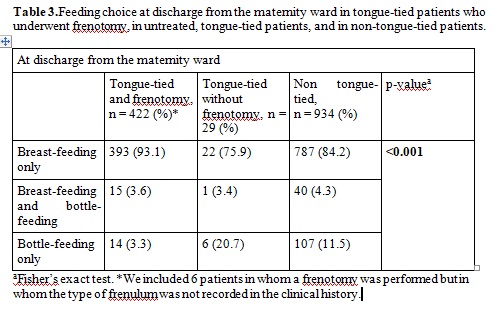
Frenotomy was performed in 422 patients (30.5% of our neonates, 93.5% of tongue-tied neonates) (Table 2). Twenty-nine parents declined the frenotomy. Of those who underwent the procedure, 402 improved (95.2%) according to the LATCH breastfeeding charting system. All the interventions were performed without significant incidents other than ten cases of minimal bleeding that ceased with pressure with a gauze and a case that required stitches. Rates of breastfeeding, bottle feeding and of mixed breastfeeding at discharge are shown in Table 3. Neonates with treated ankyloglossia had a significantly higher rate of
exclusive breastfeeding than neonates without ankyloglossia and higher than neonates with untreated ankyloglossia (p <0.001). The simple odds ratio comparing rates of exclusive breastfeeding at discharge between frenotomized newborns against non-treated tongue-tied infants was 7.69 (CI 95% 2.69-21.95, p <0.001) in favor of frenotomized infants. When
performing a multivariate logistic regression, the protective effect of frenotomy continued regardless of the other variables analyzed. Even though having breastfed before seems to protect breastfeeding regardless of the presence of ankyloglossia, the difference is not significant (see Table 4).
Discussion:
With the increased popularity of breastfeeding in the last decades, there has been a resurgence of interest in ankyloglossia, especially since the 1990’s, when the terms “tongue-tie” and “frenotomy” reappeared in the literature (Hall et al., 2005; Segal et al., 2007; Messner et al., 2000; Knox, 2010; Ingram et al., 2015). Breastfeeding has overwhelming benefits both for the mother and the infant, for which it is important toaddress any condition that may impair breastfeeding (Edmunds et al., 2011; WHO, 2021).
The World Health Organization (WHO) recommends exclusive breastfeeding for the first six months and breastfeeding with complementary foods up to 2 years of age or beyond (WHO, 2021). Nowadays, approximately 80% of mothers in our area initiate breastfeeding. However, breastfeeding problems are common, which keeps rates of breastfeeding lower than they should be (Edmunds et al., 2011; Victora et al., 2016; Ghaheri et al., 2017).
Causes of early discontinuation of breastfeeding include apparent breast refusal, inadequate milk intake, introduction of formula supplementation with a subsequent decrease in milk production, and breast and nipple pain. Lingual function is more important than its appearance, as the thickness and elasticity of the frenulum and its effect on tongue movements vary widely. Thus, lingual function must be evaluated as well. Some tongue-ties restrict extension of the tongue beyond the lower gum and force the infant to use its jaw to keep the breast in the mouth and form a proper seal, making breastfeeding difficult (Hall & Renfrew, 2005; Ballard et al., 2002; Edmunds et al., 2011; Segal et al. 2007; Lalakea & Messner, 2003; Ricke et al., 2005; Knox, 2010; Griffiths, 2004; Schlatter et al., 2019; Ingram et al., 2015; Ghaheri et al., 2017). As previous studies have suggested, careful assessment of the lingual function and frenotomy in cases of ankyloglossia facilitate breastfeeding (Ballard et al., 2002; Edmunds et al., 2011; Hogan et al., 2005; Know, 2010; Schlatter et al., 2019; Ingram et al., 2015; Ghaheri et al., 2017; Ridgers et al., 2013). One of the most widely used tools to assess lingual function is the ATLFF (Assessment Tool for Lingual Frenulum Function) score (Hazelbaker, 1993).
While some tongue-tied infants are unable to attach to the breast, others can attach but are less efficient at breastfeeding (Hall & Renfrew, 2005; Ballard et al., 2002; Edmunds et al., 2011; Segal et al., 2007; Knox, 2010; Schlatter et al., 2019; Ingram et al., 2015; Ghaheri et al., 2017). Research has shown that between 25 and 80% of tongue-tied infants have difficulty breastfeeding (Schlatter et al., 2019; Francis et al., 2015). Even though most studies have not found any effects on bottle feeding, given the more passive efforts involved with bottle feeding, a few authors have observed that tongue-tied infants may have trouble sucking from a bottle as well (Hall & Renfrew, 2005; Ballard et al., 2002; Messner et al., 2000; Hogan et al., 2005; Ricke et al., 2005; Knox, 2010). We believe that all the newborns should be explored to rule out the presence of tongue-tie and should be offered a frenotomy as soon as possible in case of ankyloglossia (Knox, 2010; Schlatter et al., 2019).
We agree with Ricke that frenotomy should be performed before one week of age, because studies have shown that for every day of maternal pain during the initial three weeks, there is a 10 to 26% risk of cessation of breastfeeding (Segal et al., 2007; Hogan et al., 2005; Ricke et al., 2005; Schlatter et al., 2019).
The procedure used to treat ankyloglossia is a frenotomy, which is simple release or “clipping” of the frenulum with or without local anesthesia (Ballard et al., 2002; Edmunds et al., 2011; Segal et al. 2007; Lalakea & Messner, 2003; Messner et al., 2000; Hogan et al.,2005; Ingram et al., 2015). Whereas an asymptomatic lingual frenulum does not need to be treated, ankyloglossia that interferes with breastfeeding is an indication for frenotomy, a simple, safe and effective procedure in treating tongue-tie and increasing successful breastfeeding (Ballard et al., 2002; Edmunds et al., 2011; Segal et al. 2007; Hogan et al.,
2005; Griffiths et al., 2004; Ridgers et al., 2013; Dollberg et al., 2006; Finigan, 2009). Midwives already performed neonatal frenotomies in the 19 th century. In the 1960’s, frenotomies were performed less frequently due to the increase of bottle feeding. Nowadays there is controversy in regards to the need to perform it and its optimal timing: performing it in infancy does not require general anesthesia and may prevent feeding, speech or other problems (Edmunds et al., 2011; Lalakea & Messner, 2003; Messner et al., 2000; Knox, 2010; Messner & Lalakea, 2000; Rowan-Legg, 2015; Francis et al., 2015; Webb et al.,
2013). Potential adverse effects include bleeding, infection, ulceration, pain, damage to the tongue and submandibular ducts, and recurrence, although most recent studies report little discomfort and few adverse effects (Hall & Renfrew, 2005; Ballard et al., 2002; Edmunds et al., 2011; Segal et al., 2007; Hogan et al., 2005; Knox, 2010; Griffiths, 2004; Ingram et al., 2015; Ridgers et al., 2013; Dollberg et al., 2006; Masaitis & Kaempf, 1996; NICE, 2021). We had ten cases of bleeding that required only pressure and one that required stitches.
Even though there are not clinical trials that demonstrate the advantage of performing postoperative “tongue exercises”, we recommend them mainly to avoid reappearance of the tongue-tie during scarring (Pransky et al., 2015). Tongue movements
during breastfeeding also prevent re-adhesion (Knox, 2010). Support from a lactation specialist is recommended regardless of the performance of a surgical division (Segal et al.,2007; Messner et al., 2000; Hogan et al., 2005; Ricke et al., 2005; Ingram et al., 2015; Dollberg et al., 2006; Geddes et al., 2008; Power & Murphy, 2015). Like in Ballard and Hogan’s observations, we observed a dramatic improvement in 95.2% of cases in terms of decreased maternal nipple pain and/or better latch onto the
breast. Sometimes improvement is not immediate because sore or traumatized nipples may take 24 to 72 hours to heal and the baby may need time to re-learn suckling (Ballard et al., 2002). Ghaheri’s prospective cohort study found an immediate improvement following frenotomy but also that breastfeeding continued to improve over the first month post-procedure both in anterior and in posterior tongue-ties (Ghaheri et al., 2017). Schlatter evaluated breastfeeding at the age of 2.5 weeks and found that only 13% of frenotomized neonates continued to have breastfeeding problems following the procedure (Schlatter et
al., 2019). Messner found that 83% of infants with ankyloglossia were breastfed for at least two months, compared with 92% of control infants (Messner et al., 2000). In our case, 415 of 451 (92.0%) neonates with ankyloglossia were exclusively breastfed at discharge, and the percentage was higher in frenotomized infants, probably because mothers who accept a frenotomy are likely more prone to breastfeeding, and for this reason they may also ask for more support from our nurses and IBCLC consultants.
We found that the rate of exclusive breastfeeding at discharge was higher among tongue-tied infants than non tongue-tied infants (Table 1). When comparing treated and untreated infants, the rates of exclusive breastfeeding at discharge were significantly higher in favor of frenotomy (Table 3), and such findings remained after correcting those rates by multivariate logistic regression analysis taking into account other independent variables such as gender, birth mode, prematurity, birth weight, maternal age, and previous breastfeeding experience. We took into account whether the mother had breastfed a previous baby; however, we did not analyze for how long or if exclusively. These results seem to indicate that the performance of a frenotomy in tongue-tied infants helps establish breastfeeding. However, we could not draw conclusions from the effect of performing a
frenotomy because we did not have a formal control group. Treated and untreated tongue-tied infants could have not been homogeneous in their interest to breastfeed even though they were in terms of the variables we analyzed.
One of the strong points of this study was the large number of cases. This is, as far as we know, the largest study published to date, which took place at one single center and which was carried out by a small team of three neonatologists. Our study also has limitations. The main limitation is the lack of a formal control group, because we offered the frenotomy to all tongue-tied patients and most parents accepted it. Due to the low risk of frenotomy and the risks of early weaning, we did not find it ethical to have a control group. The group of mothers with tongue-tied neonates, despite being homogeneous with non tongue-tied infants in regards to the variables we measured, may not be homogeneous in terms of motivation to breastfeed. This could justify the higher breastfeeding rate among mothers in the ankyloglossia group. Motivation for breastfeeding may be even more
relevant among mothers who refused frenotomy, for which comparisons between 29 untreated infants must be interpreted cautiously. Parents who refused a frenotomy could be less motivated for breastfeeding, or breastfeeding could not be their first feeding choice, for which they preferred not to do any intervention. Another limitation is that we measured
short-term improvement in terms of maternal nipple pain by asking the mothers if they felt less pain after the procedure but we did not use any quantitative measure of pain. We used no quantitative measure of infant latch onto the breast but trusted our staff’s observation of latching onto the breast. Neither the observer nor the mother were blinded, because the objective of our study was to describe our current practice, not to demonstrate the effectiveness of frenotomy. The mother was confident that frenotomy would solve her breastfeeding problems, and witnessing the procedure may have conditioned her immediate
perception of the feed. All the parents were informed of the presence of ankyloglossia, which could have influenced them to believe there would be problems breastfeeding.
However, a strength is that our multivariate regression took into account other factors that have been associated with difficulties with breastfeeding, such as lack of breastfeeding experience, prematurity, low birth weight or giving birth by cesarean (Hazelbaker, 1993), and the only factor independently associated with breastfeeding was frenotomy. The intervention took place before the establishment of breastfeeding, and since sucking improves during the first days and weeks, the improvement could have been erroneously attributed to the intervention (Hall & Renfrew, 2005). However, since breastfeeding difficulties can lead to early weaning (Ghaheri et al., 2017), we preferred to perform the intervention as early as possible.
Conclusions:
To summarize, ankyloglossia is a prevalent anomaly that may alter successful breastfeeding, mainly by causing maternal nipple pain and ineffective latch onto the breast. Frenotomy is a simple, safe, effective procedure that may help increase the breastfeeding rate at discharge in tongue-tied neonates. We need to analyze our group to look for the duration of breastfeeding.


References:
- Ballard, J. L., Auer, C. E., & Khoury, J. C. (2002). Ankyloglossia: assessment, incidence, and effect of frenuloplasty on the breastfeeding dyad. Pediatrics, 110(5), e63. https://doi.org/10.1542/peds.110.5.e63
- Coryllos, E.W., Genna, C.W., & Salloum, A.C. (2004). Congenital tongue-tie and its impact on breastfeeding. American Academy of Pediatrics. Section on breastfeeding. https://www.researchgate.net/publication/301346077_Congenital_tongue-
tie_and_its_impact_on_breastfeeding - Dollberg, S., Botzer, E., Grunis, E., & Mimouni, F. B. (2006). Immediate nipple pain relief after frenotomy in breast-fed infants with ankyloglossia: a randomized, prospective study. Journal of pediatric surgery, 41(9), 1598–1600.
https://doi.org/10.1016/j.jpedsurg.2006.05.024 - Edmunds, J., Miles, S. C., & Fulbrook, P. (2011). Tongue-tie and breastfeeding: a review of the literature. Breastfeeding review : professional publication of the Nursing Mothers' Association of Australia, 19(1), 19–26.
- Finigan, V. (2009). ‘It's on the tip of my tongue’. Evaluation of a new frenulotomy service in Northern England. MIDIRS Midwifery Digest, 19(3), 396-400. Francis, D. O., Krishnaswami, S., & McPheeters, M. (2015). Treatment of ankyloglossia and breastfeeding outcomes: a systematic review. Pediatrics, 135(6), e1458–e1466. https://doi.org/10.1542/peds.2015-0658
- Geddes, D. T., Langton, D. B., Gollow, I., Jacobs, L. A., Hartmann, P. E., & Simmer, K. (2008). Frenulotomy for breastfeeding infants with ankyloglossia: effect on milk removal and sucking mechanism as imaged by ultrasound. Pediatrics, 122(1), e188–e194. https://doi.org/10.1542/peds.2007-2553
- Ghaheri, B. A., Cole, M., Fausel, S. C., Chuop, M., & Mace, J. C. (2017). Breastfeeding improvement following tongue-tie and lip-tie release: A prospective cohort study. The Laryngoscope, 127(5), 1217–1223. https://doi.org/10.1002/lary.26306
- Griffiths, D. M. (2004). Do tongue ties affect breastfeeding?. Journal of human lactation :official journal of International Lactation Consultant Association, 20(4), 409–414. https://doi.org/10.1177/0890334404266976
- Haham, A., Marom, R., Mangel, L., Botzer, E., & Dollberg, S. (2014). Prevalence of breastfeeding difficulties in newborns with a lingual frenulum: a prospective cohort series. Breastfeeding medicine : the official journal of the Academy of
Breastfeeding Medicine, 9(9), 438–441. https://doi.org/10.1089/bfm.2014.0040 - Hall, D. M., & Renfrew, M. J. (2005). Tongue tie. Archives of disease in childhood, 90(12), 1211–1215. https://doi.org/10.1136/adc.2005.077065
- Hazelbaker, A.K. (1993). The Assessment Tool for Lingual Frenulum Function: Use in a Lactation Consultant Private Practice. Pasadena, CA: Pacific Oaks College.
- Hogan, M., Westcott, C., & Griffiths, M. (2005). Randomized, controlled trial of division of tongue-tie in infants with feeding problems. Journal of paediatrics and child health, 41(5-6), 246–250. https://doi.org/10.1111/j.1440-1754.2005.00604.x
- Ingram, J., Johnson, D., Copeland, M., Churchill, C., Taylor, H., & Emond, A. (2015). The development of a tongue assessment tool to assist with tongue-tie identification. Archives of disease in childhood. Fetal and neonatal edition, 100(4), F344–F348. https://doi.org/10.1136/archdischild-2014-307503
- Jensen, D., Wallace, S., & Kelsay, P. (1994). LATCH: a breastfeeding charting system and documentation tool. Journal of obstetric, gynecologic, and neonatal nursing : JOGNN, 23(1), 27–32. https://doi.org/10.1111/j.1552-6909.1994.tb01847.x
- Knox I. (2010). Tongue Tie and Frenotomy in the Breastfeeding Newborn. NeoReviews, 11(9), e513-e519. https://doi.org/10.1542/neo.11-9-e513.
- Lalakea, M. L., & Messner, A. H. (2003). Ankyloglossia: does it matter?. Pediatric clinics of North America, 50(2), 381–397. https://doi.org/10.1016/s0031-3955(03)00029-4
- Masaitis, N. S., & Kaempf, J. W. (1996). Developing a frenotomy policy at one medical center: a case study approach. Journal of human lactation : official journal of International Lactation Consultant Association, 12(3), 229–232. https://doi.org/10.1177/089033449601200321
- Maya-Enero, S., Pérez-Pérez, M., Ruiz-Guzmán, L., Duran-Jordà, X., & López-Vílchez, M. Á. (2021). Prevalence of neonatal ankyloglossia in a tertiary care hospital in Spain: a transversal cross-sectional study. European journal of pediatrics, 180(3), 751–757. https://doi.org/10.1007/s00431-020-03781-7
- Messner, A. H., & Lalakea, M. L. (2000). Ankyloglossia: controversies in management. International journal of pediatric otorhinolaryngology, 54(2-3), 123–131. https://doi.org/10.1016/s0165-5876(00)00359-1
- Messner, A. H., Lalakea, M. L., Aby, J., Macmahon, J., & Bair, E. (2000). Ankyloglossia: incidence and associated feeding difficulties. Archives of otolaryngology–head & neck surgery, 126(1), 36–39. https://doi.org/10.1001/archotol.126.1.36
- National Institute for Health and Care Excellence, NICE. (n.d.). Division of anklyloglossia (tongue tie) for breastfeeding. https://www.nice.org.uk/sharedlearning/division-of-ankyloglossia-tongue-tie-for-breastfeeding
- Power, R. F., & Murphy, J. F. (2015). Tongue-tie and frenotomy in infants with breastfeeding difficulties: achieving a balance. Archives of disease in childhood, 100(5), 489–494. https://doi.org/10.1136/archdischild-2014-306211
- Pransky, S. M., Lago, D., & Hong, P. (2015). Breastfeeding difficulties and oral cavity anomalies: The influence of posterior ankyloglossia and upper-lip ties. International journal of pediatric otorhinolaryngology, 79(10), 1714–1717.
https://doi.org/10.1016/j.ijporl.2015.07.033 - Ricke, L. A., Baker, N. J., Madlon-Kay, D. J., & DeFor, T. A. (2005). Newborn tongue-tie: prevalence and effect on breast-feeding. The Journal of the American Board of Family Practice, 18(1), 1–7. https://doi.org/10.3122/jabfm.18.1.1
- Ridgers, I.., McCombe, K., McCombe, A. (2013). A tongue-tie clinic and service. British Journal of Midwifery, 17(4), 230-233.
https://doi.org/10.12968/bjom.2009.17.4.41671 - Rowan-Legg, A. (2015). Ankyloglossia and breastfeeding. Paediatrics & child health, 20(4), 209–218. https://doi.org/10.1093/pch/20.4.209
- Schlatter, S. M., Schupp, W., Otten, J. E., Harnisch, S., Kunze, M., Stavropoulou, D., & Hentschel, R. (2019). The role of tongue-tie in breastfeeding problems – A prospective observational study. Acta paediatrica (Oslo, Norway : 1992), 108(12),
2214–2221. https://doi.org/10.1111/apa.14924 - Segal, L. M., Stephenson, R., Dawes, M., & Feldman, P. (2007). Prevalence, diagnosis, and treatment of ankyloglossia: methodologic review. Canadian family physician Medecin de famille canadien, 53(6), 1027–1033.
- Victora, C. G., Bahl, R., Barros, A. J., França, G. V., Horton, S., Krasevec, J., Murch, S., Sankar, M. J., Walker, N., Rollins, N. C., & Lancet Breastfeeding Series Group (2016). Breastfeeding in the 21st century: epidemiology, mechanisms, and lifelong effect. Lancet (London, England), 387(10017), 475–490. https://doi.org/10.1016/S0140-6736(15)01024-7
- Webb, A. N., Hao, W., & Hong, P. (2013). The effect of tongue-tie division on breastfeeding and speech articulation: a systematic review. International journal of pediatric otorhinolaryngology, 77(5), 635–646. https://doi.org/10.1016/j.ijporl.2013.03.008 World Health Organization (WHO). (n.d.). Breastfeeding. ttps://www.who.int/nutrition/topics/exclusive_breastfeeding/en/


